According to new findings, a yeast fungus found in cheese and other foods can wreak havoc on the bowels of people with Crohn’s disease. In a study published Thursday, researchers found evidence that Crohn’s patients are more likely to carry this yeast than people without the disease and that this yeast is related to the slow-healing intestinal wounds that patients usually have. If valid, the findings could lead to new treatments and preventative measures for chronic and painful illness.
Crohn’s is one of the best known versions of inflammation intestinal disease (IBD). There is no clear cause of IBD, but genetics and immune system dysfunction are suspected to play an important role. Patients experience a wide range of gastrointestinal symptoms mostly caused by chronic inflammation of the gut, which come and go as outbreaks of the disease. These include diarrhea, fever, severe cramps, and weight loss. Although there are medications that can control the symptoms Diets to help people avoid possible triggers for an episode, few patients experience sustained remission.
Researchers at the Cleveland Clinic and elsewhere have been studying Crohn’s for a while hoping to find something that can help explain how and why the gut becomes so damaged in these patients. His new research, published in Science, he points to a possible culprit: a fungus called Debaryomyces hansenii.
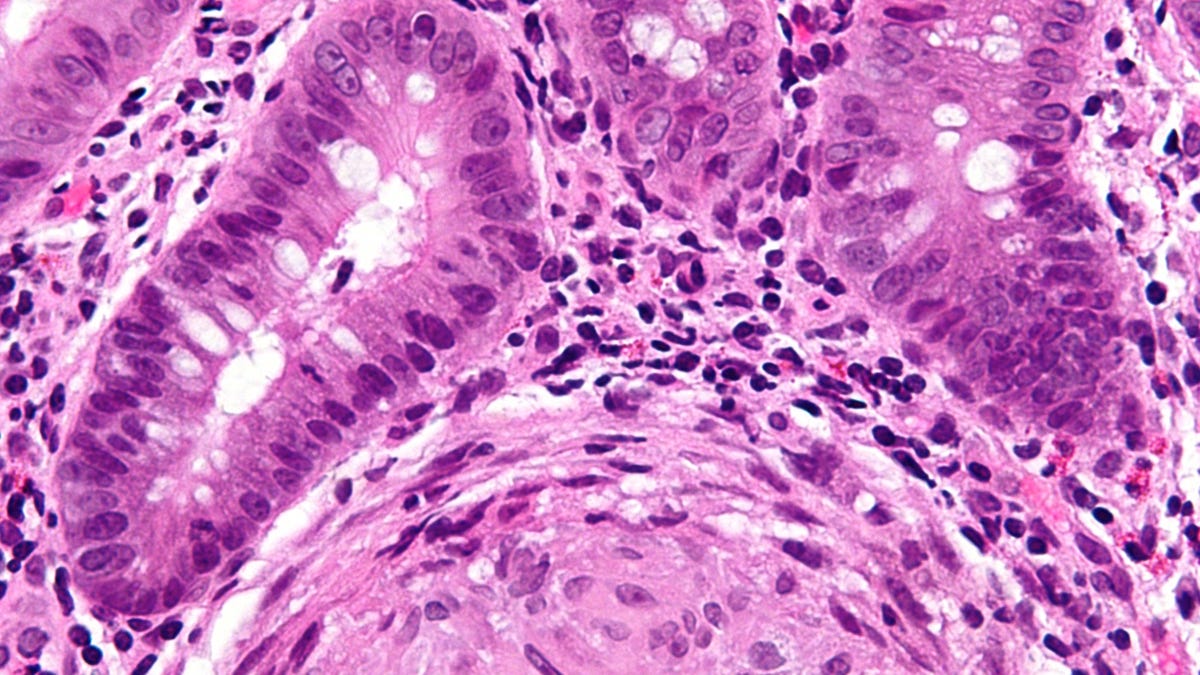
The scientists studied mice that were made to develop Crohn’s-like symptoms, as well as biopsied samples of intestinal tissue from people diagnosed with Crohn’s. Between the two groups, they found a lot of D. hansenii around injured or inflamed tissue, but not in samples taken from healthy people or in non-inflamed tissue from Crohn’s patients.
G / O Media may receive a commission
They found fungi in all seven samples taken from a group of Crohn’s patients, for example, but only in one of 10 healthy controls used as a comparison. They also found evidence that this yeast was directly related to the slow healing of intestinal wounds in mice. And when they took samples of the fungi of a Crohn’s patient or sick mice and gave them to a new group of healthy mice, their ability to heal intestinal wounds worsened. This effect was reversed when antifungal treatment was performed on mice.
All the combined findings, according to the researchers, meet Koch’s postulates, a criterion scientists use to show that a specific microbe is causing a specific set of symptoms. In other words, it suggests this D. hansenii he is not only a harmless spectator lying in the bowels of these patients, but an active source of trouble. At this time, it is not known how patients might be exposed to fungi or whether yeast-rich foods, such as cheese, could be a source.
“It simply came to our notice then D. hansenii inhibits the repair of ulcers in the inner lining of the gut in patients with Crohn’s disease, “study author Thaddeus Stappenbeck, chair of the Department of Inflammation and Immunity at the Cleveland Clinic, told Gizmodo Lerner Research Institute. “This feature is a hallmark of many Crohn’s patients with moderate to severe disease.”
According to his current theory, fungal infection does not cause Crohn’s disease itself, Stappenbeck added. Rather, it “perpetuates the disease that has already begun.”
The findings are still based on a small group of patients and animal research, so they should not be seen as definitive proof of team theory. And even if they are right, Crohn’s and IBD in general will remain one complex disease with symptoms that cannot be fully explained by a single microbe. In the mice they studied, for example, the excess fungus only occurred after the mice received antibiotics. There is other research pointed out to antibiotics as a possible risk factor for Crohn’s, as they can alter the delicate microscopic environment of our gut, called the gut microbiome.
If future research continues to show a strong link between Crohn’s and D. hansenii, however, could lead to important new treatments and strategies for managing the disease. “For patients with D. hansenii in their ulcers, we imagine trying antifungal drugs, “Stappenbeck said.” We hope this will also encourage the development of antifungals with fewer side effects. “
Another area of research could involve the orientation of how D. hansenii it seems to cause intestinal inflammation in the body, through a protein called CC5 produced by some immune cells. And, since yeast is commonly found in cheeses and other processed foods, it could be worthwhile for patients in general to avoid these foods, the researchers say. The team also plans to continue studying how yeast interacts with the gut microbiome and immune system of people with Crohn’s.
This article has been updated with comments from one of the study’s authors.