If anything the pandemic has revealed are the weaknesses of the health care system. Lack of technologies, protective equipment, production capacity, lack of supply problems; the collapse of primary care due to the lack of resources and professionals in the ICU; the vulnerability of tracking and surveillance structures to control the epidemic; the lack of coordination between the Autonomous Communities, which has led to a slow and heterogeneous response, and the absence of long-term prevention and planning strategies are some of them. But what to do and how to improve management at a critical time?
In December, more than 300 clinicians, academics, economists and jurists published a manifesto proposing the creation of an independent institution to evaluate health benefits. That is, a public agency with organic status that assesses and recommends the entry into the system of new drugs, medical devices, diagnostic tests and trials, technologies and surgical interventions, after a cost-effectiveness analysis by a committee of multidisciplinary experts -specialists, biostatisticians, health economists, ethicists, patient organizations, epidemiologists, pharmacologists-, explain Ruth Puig Peiró and Pilar Pinilla Domínguez, respectively, vice president and member of the Association of Health Economics (AES ), an entity that organized a subsequent debate, in February. It would be like an Airef, but sanitary, they illustrate.
The idea is to evaluate the cost-effectiveness of all health benefits, from drugs to medical devices.
“In Spain, health management and financing is much more politicized. Decision-making is done from within the ministry. [de Sanidad]”There is no protection, guarantees, to minimize these interferences, nor a homogeneous system, and this can create inequalities in access and a significant lack of coordination”, argues Puig, who worked at the Catalan Health Service (CatSalut).
The country has the Spanish Network of Agencies for the Evaluation of Health Technologies and Benefits (Redets), but does not examine the cost of drugs, says Pinilla, which is done through RevalMed. “These agencies exist at the regional level, are managed as they can and depend a lot on political management at the moment,” adds Puig. That is why they are proposing the creation of a HispaNice, emulating the British model, the National Institute for Health and Care Excellence (Nice), which has been operating since 1999 and the recommendations are legally binding. In Germany, France, the USA, Canada or Australia the suggestions of these agencies are not.
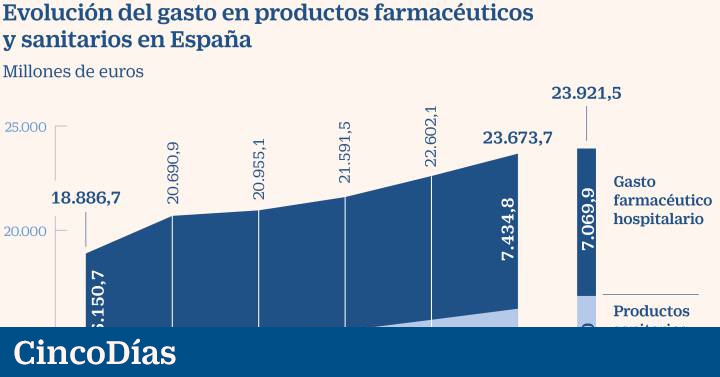
The economist promoting the document, Guillem López Casasnovas, a professor at Pompeu Fabra University (UPF) and also a member of AES, urges work in two areas: streamlining current spending and prioritizing the future. “What has grown in recent years in double digits is hospital pharmaceutical spending due to the poorly resolved tension between the hospital pharmacy and clinicians. It is not rationalized which is the best option and which is susceptible to follow-up by the rest. of centers “, he points out.
And with regard to future spending, he adds, “Someone has to look at whether the incremental benefit of the new technology, drug, or indication over the existing one corresponds to the additional costs.” López is in favor of copying the American ICER (Institute for Clinical and Economic Review), which focuses on the analysis of effectiveness. “It requires fewer people, the existing agency network can be used and only a law needs to be passed that protects these actions,” he argues. The investment (not calculated) would be made with European funds and would be self-financed with the fees it charges the industry for its services.
For the employer Farmaindústria, “the economic evaluation is necessary in the process of price and financing of new medicines and it is up to the State to decide who makes it. The important thing is that it is done according to an objective, transparent procedure. , participatory and agile “.
Digitization, another of the challenges
The digitization of the healthcare system is key to the incorporation of precision personalized medicine and to achieving patient-centered preventive, diagnostic and therapeutic care. This is stated in a recent report published by the Roche Institute Foundation, which includes 50 recommendations in five areas to advance its implementation, improve management and reduce costs.
The document, by a group of specialists and experts from different areas, proposes the need to promote technological innovation, have an interconnected infrastructure and establish actions to ensure governance and regulation under the values of bioethics. .
In addition to ensuring the organization, standardization and interoperability of data, its security, and improve the training of health professionals, managers and system actors. This will promote, according to the report, a model of preventive care, public health, biomedical research, management and patient participation in decision-making.