In another setback in decades of scientific research on HIV vaccine, a candidate for Johnson & Johnson’s HIV vaccine was unable to reduce the risk of infection in a clinical trial among women in South Africa. The future vaccine uses the same underlying technology that is successfully used for COVID-19 and Ebola viruses, but this recent high-profile failure is another example of the immense challenge of creating an HIV vaccine.
The trial, called Imbokodo, was sponsored by the Bill & Melinda Gates Foundation and the U.S. National Institutes of Health. It included more than 2,600 women living in five African countries where women and girls are at high risk for HIV infection.
The researchers said the vaccine was safe, but ultimately the effectiveness was only 25%, meaning people who received the vaccine had a slightly lower risk of developing HIV, but the difference was so small that the result could be calculated at random.
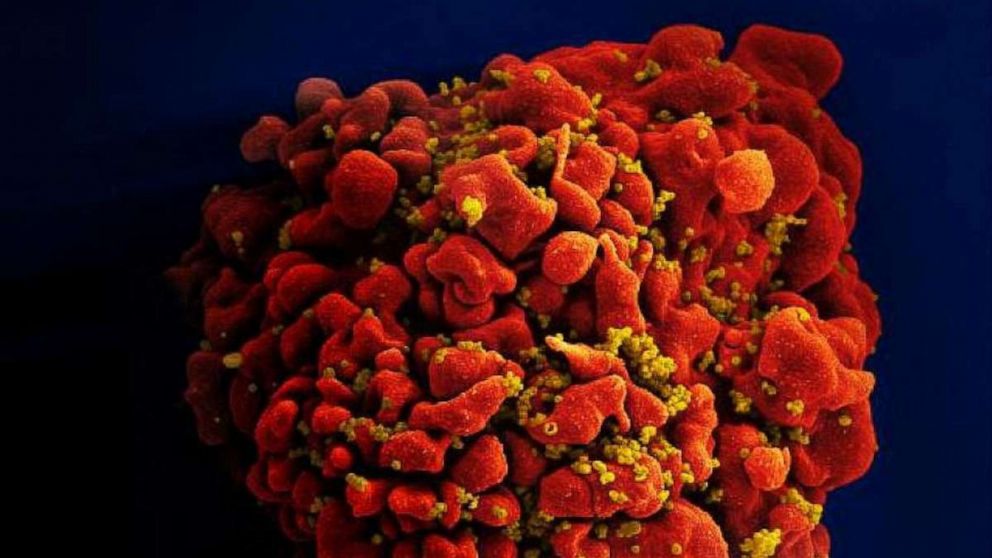
Leading scientists, including Dr. Anthony Fauci, have been looking for an effective HIV vaccine since the virus, which attacks the immune system and leads to a disease called AIDS if left untreated, was first identified in the 1980s. Today, nearly 38 million people live with HIV worldwide. Although effective treatments can now help HIV-infected people live long and healthy lives, there is still no vaccine that can prevent the infection.
Still, scientists say they don’t give up.
“The development of a safe and effective vaccine to prevent HIV infection has proven to be a formidable scientific challenge,” Fauci said in prepared statements. “While this is certainly not the result of the study we had hoped for, we must apply the knowledge learned from the Imbokodo trial and continue our efforts to find a vaccine that protects against HIV.”
“The challenges associated with the development of an HIV vaccine are unprecedented in the history of vaccinology. After 40 years of global efforts, we still do not have an HIV vaccine,” said Dr. Dan Barouch, director of the Virology and Vaccines Center. Research at Beth Israel Deaconess Medical Center.
“This trial was not done at home, hopefully it will guide the field of HIV to move forward,” said Barouch, whose lab significantly contributed to the initial development of the research vaccine.
Despite the setback, the Imbokodo trial showed that the vaccine was safe among people who received it, a hopeful sign. Imbokodo means “rock” in the South African language isiZulu, referring to a proverb about the strength and community of women.
“We are very grateful to the women who volunteered for the Imbokodo study and to our partners, including front-line people, who contribute every day to this enduring quest to make HIV history.” Dr. Paul Stoffels, vice chairman of the executive committee and scientific director of Johnson & Johnson, said in prepared statements.
Johnson & Johnson’s HIV vaccine uses the same underlying “viral vector” technology that is used in its current COVID-19 vaccine. Scientists say the recent failure has no bearing on the technology itself, which has been used successfully for other viruses, including Ebola and SARS-CoV-2, the virus that causes COVID-19. Rather, HIV itself is a unique virus. It bypasses the body’s immune system, making it very difficult to create a vaccine that generates immunity to the infection.
HIV activists and scientists say this result should not slow down other efforts to find an effective HIV vaccine.
“It is very disappointing that this particular vaccine candidate has not worked on this trial, but the trial has been well conducted and has received a response quickly. HIV remains a global threat and a vaccine is still needed. safe, effective and accessible to help contribute “to curb new infections and provide a lasting end to the pandemic,” Mitchell Warren, executive director of the organization advocating for the prevention of HIV AVAC, said in prepared statements.
Another end-of-phase trial called Mosaic will continue, which uses a slightly different vaccine approach and is being tested among men who have sex with men and transgender people in Europe and North America. Another study called PrEPVacc combines candidates for the HIV vaccine with a once-a-day pill called PrEP, which reduces the risk of HIV infection. Meanwhile, Moderna has said it will begin early-stage clinical trials of its own candidate for the HIV vaccine, which uses its mRNA technology, this year.
“This is by no means the end of the search for an HIV vaccine,” Warren said.