Medical experts have warned for months that the United States lags far behind other countries in research on the evolution of coronavirus, both in speed and overall focus. In early December, the discovery of a faster-spreading variant of COVID-19 in the UK gave urgency to the need for genetic sequencing to help determine whether treatment regimens and vaccines remain effective against new mutations in the virus.
In the United States, the first case of the British variant B.1.17 was discovered in Colorado in December, and since then at least 15 states have identified cases of the strain. Public health experts say it is likely to spread here unseen, a victim of the country’s long-delayed COVID-19 sequencing campaign, and warned that other new variants of its own production could also mutate without anyone noticing. know.
According to an analysis by the Broad Institute, of the global GISAID Initiative database, it is estimated that the United States will lag behind more than 30 nations in its sequencing effort.
But Colorado, where the first case of the UK variant with the fastest spread in the United States was found, is rushing to reverse this trend. The state has expanded staff and public health equipment to accelerate its efforts. Their labs have identified the genetic sequencing of 1,400 samples so far and aim to sequence about 200 samples a week.
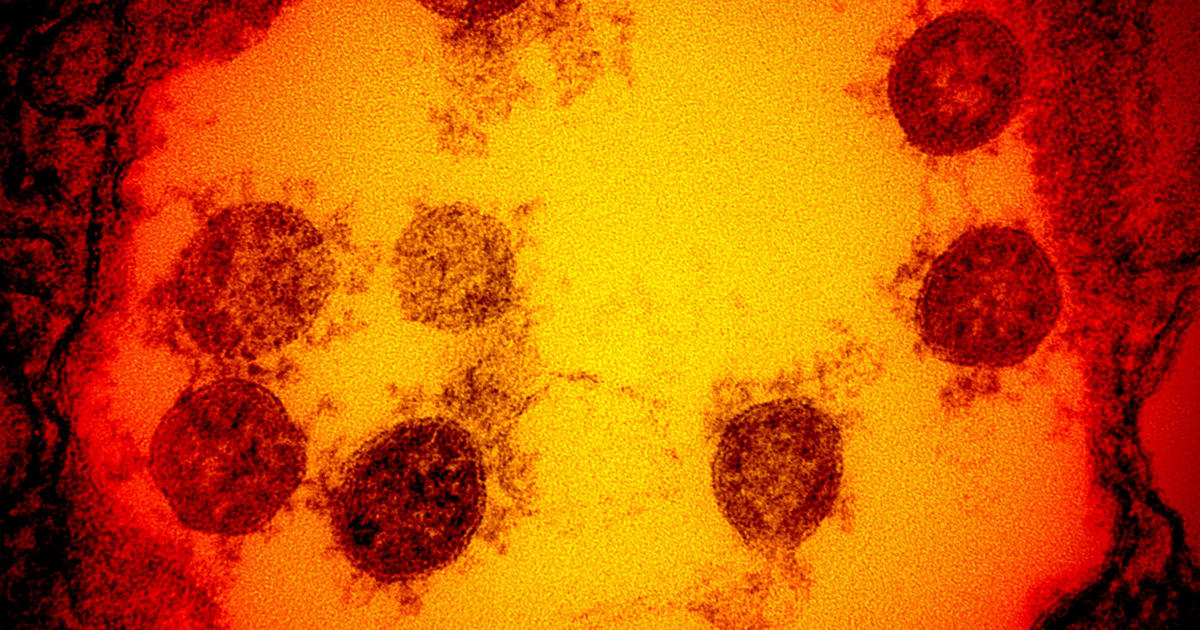
The sequencing process involves extracting and analyzing unique genetic information in a virus sample to look for mutations. These findings help public health researchers track the spread of particular variants of the disease. Although mutations are frequent and often harmless, variant B.1.17 appears to spread more easily than previous strains. Both Pfizer and Moderna have said they believe their vaccines will still be effective against it.
Even before identifying the Colorado case, state health department labs were conducting diagnostic tests that could immediately pinpoint potential samples with one of the mutations characteristic of the UK variant. Staff were also trained on new procedures to speed up the search for the fast-moving error.
Emily Travanty, scientific director of the Colorado Department of Public Health and Environment, said “it was really a bit of luck” that the sample of the first UK case in the United States arrived at her lab.
“We don’t have all the samples all over the state of Colorado, so the sample got us here and we were on the lookout, it was a little bit of luck,” Travanty said.
Some states have struggled to stay the same. The increase in coronavirus cases has forced laboratories to choose between local population diagnostic tests and virus sequencing, a process that requires many resources and can take days.
“More than anything, sequencing has been reduced to staffing,” said Kelly Wroblewski, director of infectious diseases at the Association of Public Health Laboratories (APHL). He said APHL has heard of frustrated labs with “incredibly strict” supplies used for both sequencing and other lab work.
Researchers at the University of California at Los Angeles were among those who dropped out of their sequencing work last year, amid a surge in COVID in Southern California.
“We just didn’t have the capacity,” Omai Garner, director of clinical microbiology at UCLA Health System, told CBS News.
“The people I would use for this sequencing are the same people who did the diagnostic tests,” Garner added.
When the Trump administration ends, senior Biden transition officials say stepping up sequencing work will be a top priority in funds requested in Congress as part of the president-elect’s COVID-19 bailout proposal .
In November, the Centers for Disease Control and Prevention announced it would expand its own capacity to collect and sequence coronavirus samples from health authorities across the country. Samples sent to CDC labs identified the first cases of B.1.1.7 in several states, including Texas, Indiana and Pennsylvania, state public health officials told CBS News.
This month, Illumina and LabCorp announced new CDC contracts to sequence samples of SARS-CoV-2, the virus that causes COVID-19. Illumina has since identified 51 of the first 54 cases of variant B.1.1.7 in the country.
The CDC also announced in December that it would release about $ 15 million in funding to support local sequencing efforts through the Epidemiology and Laboratory Capacity (ELC) program, which has been sent to some public health laboratories. on the front lines of the pandemic.
A spokesman for the Massachusetts State Public Health Laboratory said the agency had received $ 3.4 million in ELC funds, which had been earmarked for new staff, equipment and supplies. In Utah, officials said CARES funding and an ELC grant of about $ 176,000 had helped the state increase sequencing capacity to about 3,000 samples a day. And in Arkansas, a spokesman said his ELC money was expected to arrive “soon.”
“They, like us, are on the rise,” Travanty said of the CDC. She says CDC has now doubled the number of samples it has requested from states for its strain monitoring program.