:quality(70)/cloudfront-us-east-1.images.arcpublishing.com/adn/DEM7U6UNVCI7RJK3C2MAA3CAPM.jpg?resize=560%2C0&ssl=1)
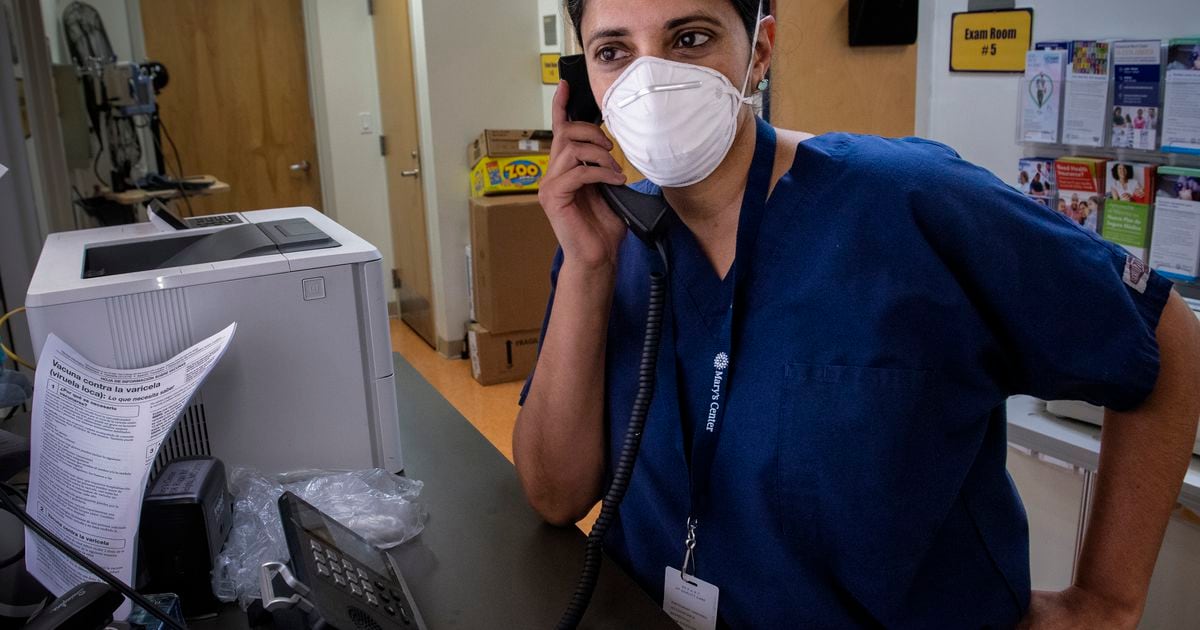
Kavita Patel, a primary care physician at the Mary’s Center in the Washington area, routinely launches perfectly good doses of coronavirus vaccine. When you open a new multidose vial, any shot that does not go in your arms that day should be ruled out.
In the last few days, he was tempted to do something different: use one of those doses that would soon be lost to boost his own immunity.
It may seem obvious, but nothing is easy when it comes to coronavirus vaccine enhancers. The Biden administration’s coronavirus working group wants to launch boosters the week of September 20th. Very soon, some experts have stated. Not soon enough, others say.
Meanwhile, officials from the Food and Drug Administration, which has regulatory authority on these matters, have warned the White House that they should initially limit the boosters to people who received the Pfizer-BioNTech vaccine because they have not yet received the data. they need. to make decisions about Modern and Johnson & Johnson vaccine drivers.
There is even a debate over whether to call a third shot a “booster” or declare it only part of the initial series of vaccinations.
“It shouldn’t be so confusing,” Patel said.
It seems that reinforcement confusion has reached epidemic proportions amid a flood of new scientific studies that are not always consistent with each other. “Getting vaccinated completely” is suddenly a mild concept. People who felt relatively bulletproof after two shots have been forced to rethink what is safe, what is risky and whether they are really protected from coronavirus, especially this summer of the delta variant, with new infections that they have gone on to an average of over 150,000 a day.
“You know what’s going on: people just do what they want,” Patel said. “I know of patients who have received reinforcement four months after their second dose.”
Reinforcement confusion dates back to August 18, when top administration doctors and President Joe Biden revealed that they wanted adults to receive a third mRNA vaccine, the Pfizer-BioNTech or Modern, eight months after receiving her second.
But the reinforcement plan is not an agreement made: it requires the approval of the FDA and the Centers for Disease Control and Prevention. Two of the top FDA regulators in recent days announced their release later this year. An FDA advisory committee is expected to discuss the reinforcement plan, specifically the Pfizer-BioNTech feature, at a Sept. 17 meeting. The FDA will then decide whether to approve the reinforcement and weigh a CDC advisory committee.
Administration officials concede that the eight-month period is somewhat arbitrary and can be modified. Biden recently introduced the possibility of speeding up the process, with boosters just five months after the end of the initial two-dose regimen.
Another peculiarity of the reinforcement plan is that there are already third gunshots, 1.33 million according to the latest CDC count, because the FDA approved in August an additional dose for people with moderate to severe immunocompromised and that they may not have mounted a sufficient immune system. answer.
“Immunocompromised” is a term that encompasses a wide range of medical conditions. There is no system for applying the eligibility rule. There is no national vaccine registry that tracks who has and has not had a vaccine. A third trait to protect against coronavirus pivots largely at the discretion of doctors and pharmacists and perhaps the persuasion of the person seeking reinforcement.
Left a bit in limbo for now, but will likely be included in the administration’s strengthening plan, eventually there are people who received the Johnson & Johnson vaccine in one shot.
That’s a lot for normal people to process.
“We went through a very confusing little guide,” said J. Stephen Morrison, director of the Center for Global Health Policy at the Center for Strategic and International Studies, a DC think tank. “People take things into their own hands.”
[How and when you should use an at-home COVID-19 test]
No one doubts that protection against mild to moderate diseases is gradually diminishing. And the delta variant replicates so quickly in a person’s nose that an infection can catch up before the immune system can deploy all of its elements that eliminate the virus. But several studies have shown that protection against serious cases, the main goal of vaccination, has been relatively constant.
Advanced cases among vaccinated individuals are usually asymptomatic and do not usually require hospitalization. However, a “mild” case may flatten a person for days and the illness may not feel mild for the person suffering from it, but recovery can occur at home, as with most cases of grip. Vaccines offer protection against all variants that have emerged so far.
This has led some critics of the reinforcement plan to argue that the administration is not following science, but guessing what science will show at some point in the future. Administration officials have effectively acknowledged this: Surgeon General Vivek Murthy has said the plan was being implemented to anticipate a possible decline in the effectiveness of the vaccine against serious diseases.
:quality(70)/cloudfront-us-east-1.images.arcpublishing.com/adn/FVNPAS6QIJH7VF6YRP7T3PYJPA.jpg?resize=560%2C0&ssl=1)
Much of the debate has focused on data from Israel, which began vaccinating and has abundant research on the effectiveness of the vaccine. Biden’s chief medical adviser for the pandemic, Anthony Fauci, on Thursday cited new studies from Israel, not yet peer-reviewed, that show a growing number of serious infections and a protective benefit against infections and serious diseases. a third shot of the Pfizer vaccine.
“There is no doubt about the dramatic data from the Israeli study that the impulses that are being made there now and that are contemplated here strongly support the justification for this approach,” Fauci said.
While acknowledging that the FDA must make the decision on whether a person will need three shots to be considered “fully vaccinated,” Fauci said he believes the three-shot regime is about to become the standard.
As public health officials debate the need for reinforcers, they are struggling with broad strategic questions about how best to end the pandemic. Is the goal to crush the virus or to adapt to it?
How much should the country rely on vaccines to control the virus, as opposed to a strategy that complements the vaccination campaign with layers of other interventions, such as the use of masks, social distancing and restrictions on meetings?
The public may need to adjust their expectations and risk tolerance. Vaccines continue to be a powerful tool in the fight against the virus, but advanced (mostly non-serious) infections have been a fact of life since the summer of 2021.
Vaccines, even augmented ones, cannot eliminate all risk of coronavirus infection, said Celine Gounder, an infectious disease specialist and epidemiologist at New York University and Bellevue Hospital.
“You won’t be able to prevent advanced infections indefinitely unless you want to increase people every three to six months, and you never will,” Gounder said.
He believed the Biden administration’s strengthening plan was premature and perhaps responded more to public concerns than to scientific ones: “This seems to only yield to anxiety about advanced infections.”
Some experts argue that boosters may make individuals more protected from infection, but these additional shots may not be the best use of a valuable resource.
There is the ethical problem of giving a third dose to people when the majority of the world’s population has not had the first. Patel is aware of this when he plans to get a third shot, which is why he would use a dose already destined to be discarded.
Morrison, on the other hand, believes the administration should pressure vaccine manufacturers to distribute more of their doses to poor, middle-income countries even though companies will make more money by selling a third dose to people in rich countries. .
The biggest challenge for the United States is the unexpected and tragic summer wave of infections, hospitalizations, and deaths, driven by the delta variant. The best way to reduce the spread of the virus is to get a first vaccine against the unvaccinated, because they are more likely to contract the virus and release it for a longer period when they are sick, according to experts.
This, in turn, can protect people more than a booster shot. Less virus means less risk, regardless of how many shots a person has had.
The Biden administration’s strengthening plan includes everyone 18 years of age or older, although younger people are much less likely to have serious illnesses. Drivers “are not irrational” for some groups of people, such as those who are immunocompromised, “but for younger people, it’s extraordinarily weird,” said William Hanage, an epidemiologist at Harvard TH Chan School of Public Health . “If you have someone who is 85% protected from hospitalization and 90% increase, it’s not really a big benefit.”
The best approach to crushing the pandemic will not be based simply on vaccines, said David Dowdy, an epidemiologist at the Johns Hopkins Bloomberg School of Public Health.
“We shouldn’t think of booster shots as our way out of the pandemic,” Dowdy said. Taking the virus seriously, he said, “it doesn’t mean everyone has to be isolated at home all the time. But it means you have to think twice about attending big events where there will be thousands of other people or celebrating parties with a lot of people without masks sharing a room for a long period of time – this kind of high-broadcast event “.
Another way of saying this is: the pandemic is not over. Being “completely vaccinated” (a dubious designation, it turns out) doesn’t mean anything goes wrong. Many people who expected the opposite may feel as if the rules for interacting with the virus continue to change and the finish line continues to drift away.
“Why should we be surprised if the target post moves?” Morrison said. “We are dealing with an incredibly cunning and pernicious virus.”
The virus continues to mutate. Although almost all new infections in America are caused by the delta variant, there are other variants appearing worldwide, including a new “variant of interest,” first identified in Colombia and called mu by the Organization. World Health. It has not gained a significant foothold in the United States.
Vaccines are also not entirely static and this could lead to a new set of confusing problems. Pharmaceutical companies are in the process of manufacturing more customized “next generation” vaccines according to the delta variant or possibly with a wide range of mutated coronaviruses.
Patel says his teammates have asked him, “Should I even get a booster or should I wait to get one of these next-generation vaccines, because it could be better?”
She advises them not to wait. She says she will get her reinforcement, because she has children at home who are not vaccinated, it’s been almost eight months since her second shot and she’s worried about the delta – “and potentially what comes after the delta”.
– – –
Laurie McGinley and Frances Stead Sellers of the Washington Post contributed to this report.