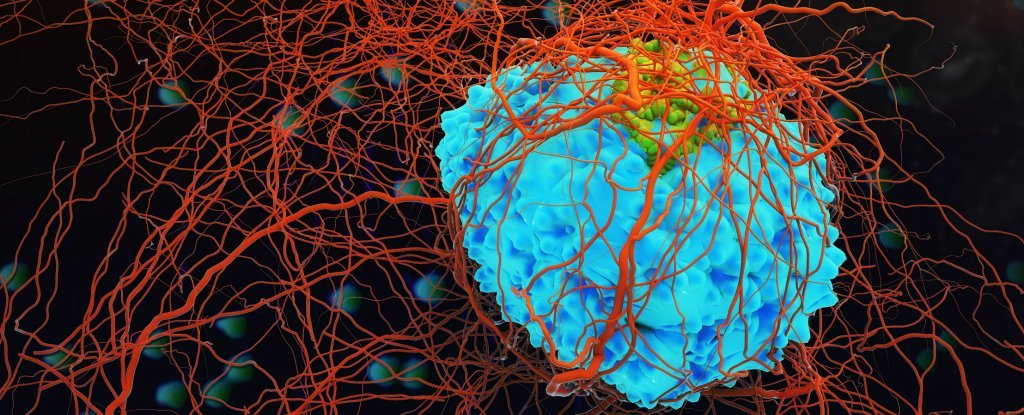
According to new research, cancer cells can hibernate like “bears in winter” when a threat such as chemotherapy treatment strikes them, apparently adopting the tactic used by some animals (although it has long been lost in humans). ) to survive during periods when resources are scarce. .
Knowing exactly how cancers evade and deal with drug treatments is an important part of working to defeat them once and for all, so understanding this hibernation behavior could play a crucial role in future research. Cancers can often return after becoming inactive or seemingly disappearing for several years after treatment.
Preclinical research on human colorectal cancer cancer cells revealed that they were able to slow down to a state of low-maintenance “drug-tolerant persistence” (DTP), which would help explain some failures in therapy and tumor relapses.
“The tumor acts as a whole organism, able to enter a state of slow division, conserving energy to help it survive,” says researcher and surgeon Catherine O’Brien of the Princess Margaret Cancer Center of Canada .
“There are examples of animals entering a reversible, slow-dividing state to withstand harsh environments. It appears that cancer cells have opted for that same state in an artisanal way for their survival benefit.”
By collecting human colorectal cancer cancer cells on a Petri dish and exposing the cells to chemotherapy, the researchers observed that the colorectal colon cancer cells went into the same state of hibernation, in a coordinated manner, when there were chemotherapy drugs. The cells stopped expanding, meaning they needed very few nutrients to continue living.
These observations also “fit a mathematical model where all cancer cells, and not a small subpopulation, have an equipotent capacity to become DTP,” suggesting that these survival strategies could be seen in all cancer cells.
The researchers also used colorectal cancer cell xenografts in different sets of mice. Once mice developed tumors of certain sizes, the researchers treated the mice with standard chemotherapy regimens. The scientists observed negligible tumor growth in mice receiving treatments for an eight-week period. When treatment was stopped, tumor growth began again.
Cancer cells extracted from tumors after a regrowth period were grafted onto different mice and re-treated. Regenerated cells continued to be sensitive to treatments and their growth stopped and began in the same way, findings consisting of cancer cells entering a DTP state.
This DTP state closely resembles a hibernation-like state called embryonic diapause in which mouse embryos travel as a sort of emergency survival mode. Embryonic diapause allows many animals, including mice, to pause embryonic development effectively until environmental conditions are more favorable.
Here cancer cells have been found doing a similar trick. Another link between the DTP state and embryonic diapause is their dependence on a biological mechanism called autophagy, in which cells are essentially eaten to find the sustenance they need. Autophagy naturally occurs in the body as a way to remove waste, but in this case cancers use it to stay alive.
“We never knew cancer cells were like hibernating bears,” says oncologist Aaron Schimmer of the Princess Margaret Cancer Center. “This study also tells us how to target these sleeping bones so they don’t hibernate and wake up to come back later, unexpectedly.”
“I think this will turn out to be a major cause of drug resistance and explain something we didn’t fully understand before.”
By targeting and inhibiting the autophagy process, the researchers were able to break the hibernation state (or DTP) and end the cancer cells permanently with chemotherapy. This could be one of the methods to tackle cancer tumors that are resistant to conventional treatments in the future.
Scientists already know other ways in which cancers can hide in the body, so this new study adds to a growing collection of evidence on how to take on the most drug-resistant cancer cells and approaches today. .
“This gives us a unique therapeutic opportunity,” O’Brien says. “We need to target cancer cells while they are in a vulnerable and slow state of cycling before acquiring the genetic mutations that drive drug resistance.
“It’s a new way of thinking about resistance to chemotherapy and how to overcome it.”
The research has been published in Cell.