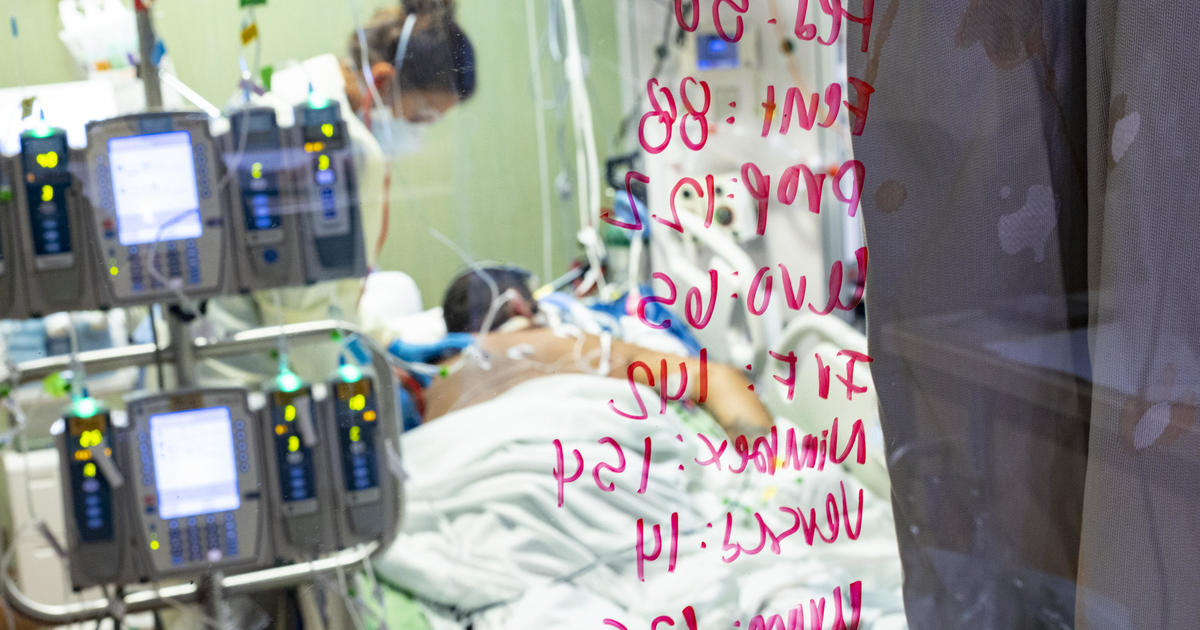
Boise, Idaho – Idaho public health leaders announced Tuesday that they have activated “crisis care standards” that allow rationing of health care in hospitals in the north of the state because there are more patients with coronavirus than institutions they can stand.
The Idaho Department of Health and Welfare enacted the move Monday in silence and publicly announced it in a statement Tuesday morning, warning residents that they might not receive the care they would normally expect if they were to be hospitalized.
The move came in the wake of confirmed cases of coronavirus status in recent weeks. Idaho has one of the lowest vaccination rates in the US
Kyle Green / AP
The state health agency cited “a severe shortage of staff and available beds in the northern part of the state caused by a massive increase in COVID-19 patients in need of hospitalization.”
The designation includes 10 hospitals and health systems in the Idaho Panhandle and north-central Idaho. The agency said its goal is to extend care to as many patients as possible and save as many lives as possible.
The move allows hospitals to allocate scarce resources, such as intensive care unit rooms, to patients most likely to survive and make other dramatic changes in the way patients are treated. Other patients will still receive care, but may be placed in hospital classrooms or conference rooms instead of traditional hospital rooms or go without medical equipment to save lives.
At Kootenai Health, the largest hospital in northern Idaho, some patients wait long periods for beds to open in the full intensive care unit, said Dr. Robert Scoggins, chief of staff. Within the ICU, a critical care nurse could supervise up to six patients with the help of two other non-critical care nurses. This is a big difference from the usual ICU nurse for a proportion of ICU patients, she said.
On Monday, Coeur d’Alene Hospital began transporting some coronavirus patients to its nearby conference center. A large classroom in the center became a COVID-19 room, with temporary dividers separating the beds. Some emergency patients are being treated in a converted portion of the emergency room lobby and the entire third floor of the hospital has also been designated for coronavirus patients.
Urgent and elective surgeries are on hold, Scoggins said, and Kootenai Health is struggling to accept any of the high-level trauma patients who would normally be transferred from smaller hospitals in the region.
Other states are preparing to take similar action if necessary. Hawaii Gov. David Ige silently signed an order last week to release hospitals and health care workers from responsibility if they are to ration health care.
State health care providers have fearfully planned to overwhelm patients at Idaho hospitals. Medical experts have said Idaho could have up to 30,000 new cases of coronavirus a week by mid-September if the current rate of infections persists.
“Crisis care standards are the last resort. It means we have exhausted our resources to the point that our health systems cannot provide the treatment and care we expect,” said the director of the health department and Idaho welfare officer Dave Jeppesen in a statement.
Kyle Green / AP
He added: “This is a decision I was keen to avoid. The best tools we have to do this are to get more people vaccinated and to put on masks indoors and in crowded public places outdoors. Please , choose to get vaccinated as soon as possible, is your best protection against hospitalization for COVID-19. “
The designation will remain in effect until there are sufficient resources (including hospital staff, beds and equipment, or a decrease in the number of patients) to provide normal levels of treatment for all.
More than 500 people were hospitalized statewide with COVID-19 on Sept. 1 and more than a third of them were in intensive care beds.
Idaho hospitals have struggled to fill vacancies in nursing, home maintenance and other health services, in part because some officials have left because they are burned by the pandemic tension and because others have been quarantined because they were exposed to COVID-19.
Late last month, Little called in 220 available medical workers through federal programs and mobilized 150 Idaho National Guard soldiers to help hospitals cope with the increase.
Two hundred of the federal workers are medical and administrative staff available through a contract with the United States General Services Administration. The U.S. Department of Defense agreed to send a 20-person medical response team to northern Idaho. Idaho National Guard soldiers will assist with logistical support, such as screenings and lab work.
On Tuesday, the governor called the measure to limit attention “an unprecedented and unwanted point in our state’s history” and urged residents to get vaccinated against coronavirus.
Data from the U.S. Centers for Disease Control and Prevention show that complete vaccination with any of the currently available coronavirus vaccines drastically reduces the risk of requiring hospitalization for a coronavirus infection.
“More Idahoans should choose to receive the vaccine so we can minimize the spread of the disease and reduce the number of COVID-19 hospitalizations, many of which involve younger Idahoans and can be prevented with safe and effective vaccines,” Little said , who is a Republican.
When the pandemic first hit Idaho in early 2020, Little ordered a partial closure of the state, ordering some companies to temporarily close or switch to retirement-style services, banning some important meetings and calling on residents who stayed home as much as possible.
The move was aimed at ensuring that hospitals are not overwhelmed by patients. Idaho was on the verge of enacting crisis care standards during a major coronavirus wave last winter, but narrowly avoided it, making it the first time the state has taken drastic action.
Little reopened the state in stages over a period of several months and has not re-imposed restrictions that limit meetings. Most companies operate normally.
State crisis guidelines are complex and provide hospitals with an ethical and legal template to use during care rationing.
According to the guidelines, patients have priority scores based on several factors that affect their likelihood of surviving a health crisis.
People who are considered most in need of care and most likely to benefit from these are on priority lists for scarce resources such as ICU beds.
Other people who need it extremely, but are less likely to survive, will be given “comfort care” to help keep them pain-free, whether they succumb to their illnesses or recover.
Other patients with serious but not life-threatening medical problems will be delayed in receiving care until resources are available.
“I hope your decision is for vaccines to work. They’re the best tool we have by far,” to prevent people from getting seriously ill with coronavirus, said Jeppesen, director of the state health department.
Demand for hospitals is likely to increase in the coming weeks as the number of cases continues to rise, Jeppesen said, so everyone should take steps to avoid the need for emergency care, if possible, leading seat belts, taking prescribed medications and reconsidering activities such as cycling that could lead to accidents.
“Be a little more careful,” he said.

