To catch cancer sooner, we need to predict who will have it in the future. The complex nature of risk forecasting has been reinforced by artificial intelligence (AI) tools, but the adoption of AI in medicine has been limited by poor performance in new patient populations and neglect for racial minorities.
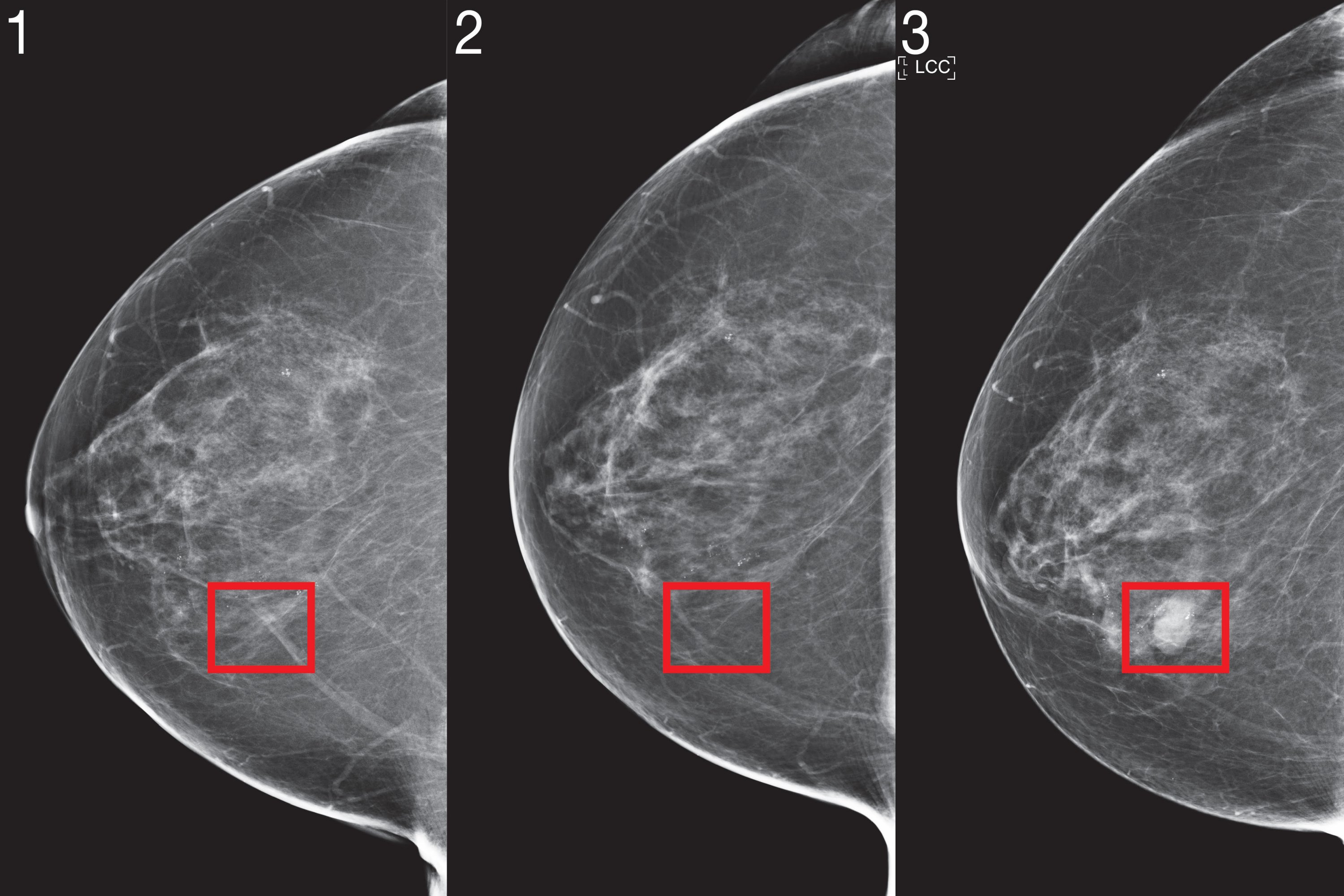
Two years ago, a team of scientists from MIT’s Computer Science and Artificial Intelligence Laboratory (CSAIL) and MIT’s Jameel Clinic (J Clinic) demonstrated a deep learning system for predicting cancer risk only through the mammography of a patient. The model showed significant promise and even improved inclusion: it was just as accurate for both white and black women, which is especially important given that black women are 43% more likely to die. for breast cancer.
But to integrate imaging-based risk models into clinical care and make them available, researchers say the models needed algorithmic improvements and large-scale validation at several hospitals to demonstrate their robustness.
To this end, they adapted their new “Mirai” algorithm to capture the unique requirements of risk modeling. Mirai jointly models a patient’s risk across multiple future time points and can optionally benefit from clinical risk factors such as age or family history, if available. The algorithm is also designed to produce predictions that are consistent between minor variances in clinical settings, such as the choice of mammography machine.
The team trained Mirai on the same data set from more than 200,000 Massachusetts General Hospital (MGH) examinations of his previous work, and validated it in MGH test sets, the Karolinska Institute in Sweden, and the Chang Gung Memorial Hospital in Taiwan. Mirai is already installed at MGH and the team’s collaborators are actively working to integrate the model into care.
Mirai was significantly more accurate than previous methods in predicting cancer risk and identifying high-risk groups in all three data sets. By comparing high-risk cohorts in the MGH test set, the team found that their model identified nearly twice as many future cancer diagnoses compared to the current clinical standard, the Tyrer-Cuzick model. Mirai was similarly accurate in patients of different races, age groups, and breast density categories in the MGH test set and in different cancer subtypes in the Karolinska test set.
“Improved breast cancer risk models allow for specific screening strategies that achieve early detection and less detection damage than existing guidelines,” says Adam Yala, a CSAIL doctoral student and lead author in a paper on Mirai that went post this week in Scientific translational medicine. “Our goal is for these advances to be part of the level of care. We are collaborating with doctors from Novant Health in North Carolina, Emory in Georgia, Maccabi in Israel, TecSalud in Mexico, Apollo in India and Barretos in Brazil to further validate the model in various populations and study how to implement it. better clinically ”.
How it works
Despite the widespread adoption of breast cancer screening, researchers say the practice is full of controversy: more aggressive screening strategies aim to maximize the benefits of early detection, while less frequent screenings aim to aim to reduce false positives, anxiety and costs for those. which will not even develop breast cancer.
Current clinical guidelines use risk models to determine which patients should be recommended for supplemental imaging and MRI. Some guidelines use age-only risk models to determine if and how often a woman should be screened; others combine multiple factors related to age, hormones, genetics, and breast density to determine further testing. Despite decades of effort, the accuracy of the risk models used in clinical practice remains modest.
Recently, risk models based on deep-learning mammography have shown promising performance. To bring this technology to the clinic, the team identified three innovations that they believe are critical to risk modeling: jointly modeling time, the optional use of non-imaging risk factors, and methods to ensure consistent performance in all clinical settings.
1. The weather
Inherent in risk modeling is learning from patients with different amounts of follow-up and assessing the risk at different times: this can determine how often tests are done, whether they should have supplemental imaging, or even consider preventative treatments.
While it is possible to form separate models for assessing risk for each time period, this approach can lead to meaningless risk assessments, such as predicting that a patient has a higher risk of developing cancer in two years than in a term of five years. . To address this, the team designed its model to predict risk at all times simultaneously, using a tool called an “additive risk layer”.
The additive risk layer works as follows: Your network predicts a patient’s risk at a given time, such as five years, as an extension of their risk at the previous time, such as four years. By doing so, your model can learn from data with varying amounts of follow-up and then produce self-consistent risk assessments.
2. Non-image risk factors
Although this method focuses primarily on mammograms, the team also wanted to use non-imaging risk factors, such as age and hormonal factors, if available, but did not require them in the moment of the test. One approach would be to add these factors as input to the model with the image, but this design would prevent most hospitals (such as Karolinska and CGMH), which do not have this infrastructure, from using the model.
For Mirai to benefit from risk factors without requiring them, the network predicts this information at the time of training and, if it is not there, can use its own predictive version. Mammograms are rich sources of health information and, by their image, many traditional risk factors, such as age and menopausal status, can be easily predicted. As a result of this design, the same model could be used by any clinic worldwide and, if they have this additional information, they can use it.
3. Constant performance in clinical settings
To incorporate deep learning risk models into clinical guidelines, the models must consistently operate in a variety of clinical settings and their predictions may not be affected by minor variations such as the machine on which the mammogram was performed. Even across a single hospital, scientists found that standard training did not produce consistent predictions before and after a change in mammography machines, as the algorithm could learn to rely on different specific cues. of the environment. To deviate from the model, the team used a file contradictory scheme where the model specifically learns mammographic representations that are invariant to the source clinical environment, to produce consistent predictions.
To test these upgrades in various clinical settings, the scientists evaluated Mirai in new test sets from Karolinska in Sweden and Chang Gung Memorial Hospital in Taiwan, and found that it performed consistently. The team also analyzed model performance in race, age, and breast density categories in the MGH test set and in cancer subtypes in the Karolinska data set, and found similar performance in all subgroups.
“African American women continue to develop breast cancer at younger ages and often in later stages,” says Salewai Oseni, a breast surgeon at Massachusetts General Hospital who did not participate in the work. “This, along with the highest case of triple negative breast cancer in this group, has led to an increase in breast cancer mortality. This study demonstrates the development of a risk model whose prediction has an accuracy “The opportunity for its clinical use is high.”
This is how Mirai works:
1. Mammography imaging is done using something called an “image encoder.”
2. Each representation of the image, as well as the view from which it came, is added with other images from other views to obtain a representation of the entire mammogram.
3. With mammography, the patient’s traditional risk factors are predicted using a Tyrer-Cuzick model (age, weight, hormonal factors). If not available, the predicted values are used.
4. With this information, the additive risk layer predicts a patient’s risk for each year for the next five years.
Improving Mirai
Although the current model does not consider any of the results of previous patient images, changes in the image over time contain a large amount of information. In the future, the team aims to create methods that can effectively use a patient’s complete imaging history.
Similarly, the team notes that the model could be further improved by “tomosynthesis,” an X-ray technique for the detection of asymptomatic cancer patients. Beyond improving accuracy, further research is needed to determine how to adapt imaging-based risk models to different mammography devices with limited data.
“We know that MRI can detect cancers before mammography and that early detection improves patient outcomes,” says Yala. “But for patients at low risk for cancer, the risk of false positives may outweigh the benefits. With improved risk models, we can design more nuanced risk detection guidelines that offer more sensitive detection, such as MRI, to patients. that they develop cancer, for best results, while reducing unnecessary detection and overtreatment for the rest. ”
“We are delighted and humble to ask ourselves whether this AI system will work for African American populations,” says Judy Gichoya, MD, MS and adjunct professor of interventional radiology and computer science at Emory University, who did not participate in work it. “We are studying this issue in depth and how to detect failures.”
Yala wrote the article on Mirai alongside MIT research specialist Peter G. Mikhael, radiologist Fredrik Strand of Karolinska University Hospital, Gigin Lin of Chang Gung Memorial Hospital, associate professor Kevin Smith of Royal Institute of Technology of KTH, Professor Yung-Liang Wan of Chang Gung. University, Leslie Lamb of MGH, Kevin Hughes of MGH, lead author and professor at Harvard Medical School Constance Lehman of MGH, and lead author and professor at MIT Regina Barzilay.
The work was supported by grants from Susan G Komen, of the Foundation for Breast Cancer Research, Quanta Computing, and the MIT Jameel Clinic. He also received support from the Chang Gung Medical Foundation grant and the Stockholm Läns Landsting HMT grant.